Abstract

Introduction:
Adolescents and young adult (AYA) patients (ages 15-39) with acute lymphoblastic leukemia (ALL) have inferior outcomes and increased treatment-related toxicity when compared to children. The use of pediatric-inspired protocols has resulted in improved outcomes in the AYA population but outcomes remain inferior to their pediatric counterparts. Hispanic patients with ALL also have inferior outcomes compared to non-Hispanic White patients. Real-world outcomes in AYA ALL patients without access to allogeneic transplant are not known, especially in Hispanic/Latino populations. Thus, in order to understand treatment outcomes with modern chemotherapy regimens in this high-risk population, we conducted a retrospective cohort analysis of all AYA ALL patients without access to allogeneic stem cell transplant at a large safety-net hospital.
Methods:
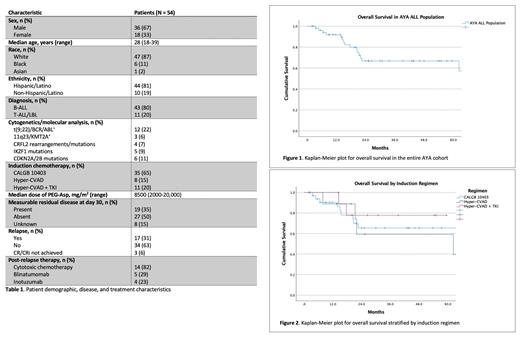
We conducted a retrospective single-center cohort analysis of ALL patients ages 18 to 39 treated at a large safety-net hospital in Dallas, TX between January 2010 and May 2021. All patients who received induction and consolidation at Parkland Health and Hospital System and did not receive an allogeneic stem cell transplant were included. We interrogated the database for demographic, laboratory, cytogenetic, and next-generation sequencing (using the Foundation Medicine platform) information as well as treatment outcomes and post-relapse therapy. Chemotherapy consisted of either Hyper-CVAD (+/- TKI) or the CALGB 10403 protocol. Data were stored in the RedCap database and SPSS analytical software was used to generate survival analysis and Kaplan-Meier plots.
Results:
We identified 54 AYA ALL patients during the designated time period, consisting of 36 males and 18 females. The median age of the cohort was 28 years, and 81% of patients were Hispanic. Twelve patients were Ph(+) and 42 patients were Ph(-); 11/12 Ph(+) patients received a TKI with induction and one patient received a TKI beginning with consolidation. Cytogenetic/FISH testing and next-generation sequencing (NGS) were performed in 42 (78%) and 13 (24%) patients respectively, with the most common aberrations noted in Table 1. Of note, NGS was not routinely performed before 2017 at our institution. Six of the 13 patients with NGS results available had Ph-like mutation signatures. The most common induction regimens used were CALGB 10403 (65%), Hyper-CVAD (15%), and Hyper-CVAD + TKI (20%). Forty-one of 49 patients (84%) with a documented day 30 bone marrow biopsy achieved a CR or CR with incomplete count recovery after induction which included 11/12 (92%) Ph(+) patients, 24/31 (77%) Ph(-) patients, and 6/6 (100%) Ph-like patients. Of the patients in CR or CRi at day 30, 27 (50%) were negative for minimal residual disease (MRD) by flow cytometry. Overall survival at 3 years for the entire cohort was 69%, and there was no statistical difference between Ph(+) and Ph(-) patients. Three-year OS was improved in patients who received Hyper-CVAD + TKI (78%) or CALGB 10403 (65%) compared to those who received Hyper-CVAD alone (59%) though this did not reach statistical significance (p=0.72).
Conclusions:
Our results underscore the ongoing outcomes disparities in the AYA and Hispanic populations, even with the use of modern pediatric-inspired and TKI-containing regimens. The 69% 3-year OS in our population is similar to that in the transplant-eligible AYA population and suggests a diminishing role for allogeneic transplant with current protocols. The high rate of Ph-like signatures on NGS in our population is consistent with the increased prevalence of these mutations in Hispanic ALL patients. Our study is limited as it is a retrospective analysis with a small sample size and represents the results of a single institution. Prospective studies are needed to determine the role of allogeneic transplant in Ph(+) and Ph-like AYA with ALL, and concerted efforts should be made to enroll Hispanic patients in these clinical trials given their high-risk biology and inferior outcomes.
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract